
OUR WORK
Care programs
OUR PROGRAMS ARE ROOTED IN CARE, BUT NEVER LIMITED TO IT.
It wasn’t long after we started our healthcare efforts in Kenya that we realized in order to truly help people, we had to think not just about treatment, but also about entire lives: families, jobs, education, and futures. It’s all connected. That’s why our programs are set up to first help people survive, and then to help them thrive.
Our process
1. FIND A NEED
Figure out what communities need, both immediately and in the long term.
2. LINK PEOPLE WITH CARE
Connect people with the healthcare systems they need and start patients on a path of sustainable health.
3. GO BEYOND CARE
Help communities sustain their own success, connect them with universal health insurance, train next generation medical professionals, and research new breakthroughs and best practices.

Explore what we do and how we do it.
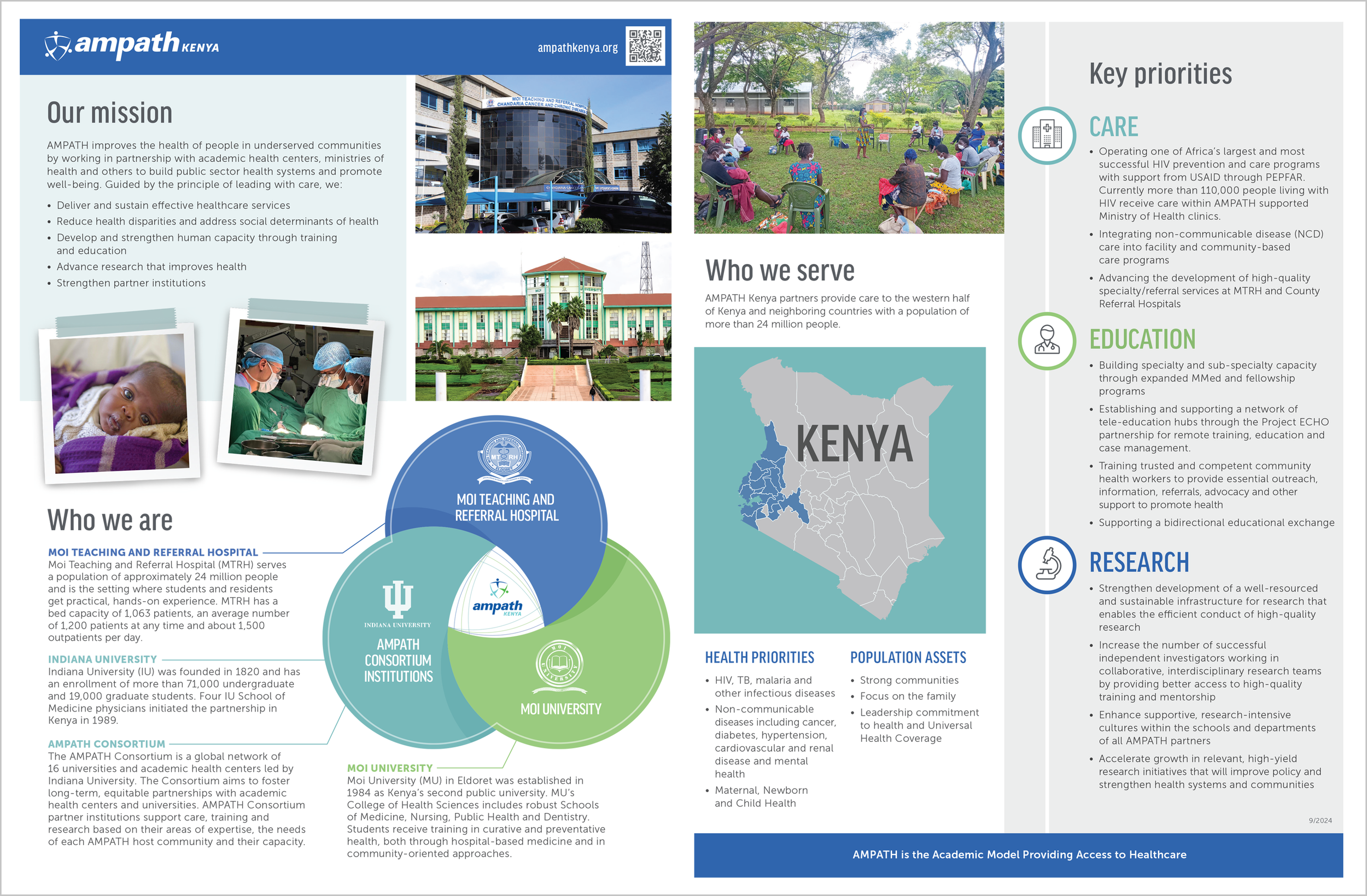
AMPATH Kenya and AMPATH Global at a glance
Flyers about AMPATH Kenya and AMPATH Global can be opened and downloaded by clicking the preview images below.

AFFORDABLE, UNIVERSAL INSURANCE FOR ALL.
We’re partnering with Kenya’s Ministry of Health and the National Health Insurance Fund to make comprehensive health insurance accessible and affordable for all Kenyans.

ELECTRONIC MEDICAL RECORDS SYSTEMS.
Recording, organizing, and sharing medical records electronically is critical to a successful healthcare system. That’s why we’ve implemented an OpenMRS as our health information system to better support patient care, follow-up care, health insurance coverage and global health research.
NURSING TEAM BUILDS CAPACITY
The AMPATH Nursing team is a collaboration between Kenyan nurses and nurses from the AMPATH Consortium to share knowledge, provide training and support quality improvement efforts to advance nursing care in western Kenya. We aim to strengthen nurses globally by building capacity on practice (care), education, and research.
MTRH Clinical Nurse Educators lead physical assessment simulations with bedside nurses in the simulation center.













